Most of the literature on minimally invasive total knee arthroplasty has been published since 2004 and I collected most of it from San Francisco AAOS Feb 2009 Meeting and Paris Sofcot Nov 2009 Meeting…
The problem, academic case study : our usual FWI candidate is much older and heavier… and still unwired !
Typical US candidate : “A 65-year-old woman with osteoarthritis of her right knee is referred by her primary care physician for orthopedic consultation.
She is healthy except for some well-controlled hypertension. She is 5 ft 5 in. tall (165 cm) and weighs 160 lb (73 kg), so her body-mass index (the weight in kilograms divided by the square of the height in meters) is 26.6.
Her arthritis is not limited to one part of her knee but is diffuse and severe.
She has minimal joint deformity and good bone quality.
For several years, she was able to control the pain in her right knee with indomethacin, but recently this has been insufficient.
An intraarticular corticosteroid injection was performed several months ago, with limited effect.
The surgeon recommends total knee arthroplasty.
The patient has a friend who has told her that his surgeon used a “minimally invasive” approach for his total knee replacement, and it went well.
The patient has investigated this approach on the Internet, and she isn’t sure what to do.
She asks her primary care physician whether he recommends that she consider “minimally invasive” surgery.”
The Clinical Problem
Osteoarthritis affects more people than any other joint disease1 and is the most common cause of long-term disability in most populations over the age of 65 years.2,3
Primary osteoarthritis is rare before the age of 40 years but becomes increasingly common each decade thereafter.1
A report from the Third National Health and Nutrition Examination Survey estimated that 37.4% of adults in the United States who are 60 years of age or older have radiographic evidence of the condition.4
Although osteoarthritis is not a life-threatening disease, the morbidity associated with this condition is considerable; 80% of patients with osteoarthritis have limitation of movement, and 25% have difficulty performing major activities of daily living.5
The economic burden of osteoarthritis may exceed $60 billion per year in the United States.1
Pathophysiology and the Effect of Therapy
The pathophysiology of osteoarthritis is complex and incompletely understood, although the hallmark of the disease is the loss of articular cartilage, with concomitant changes in the underlying bone.6,7
Many factors appear to be associated with the development of this condition, including injury, genetics, changes in tissue structure, and chondrocyte aging.7,8,9
Major trauma, such as an intraarticular fracture, clearly increases the risk of subsequent (post-traumatic) arthritis.
Research is being done to try to characterize the degree to which minor traumatic events can precipitate cartilage breakdown and degenerative joint disease,10 particularly when the injury is compounded by obesity, joint malalignment, or other predisposing factors.11
The anatomic features of osteoarthritis include loss of articular cartilage, eburnation (or “sclerosis”) of the subchondral bone, formation of osteophytes (or “bone spurs”), and the presence of degenerative subchondral cysts (Figure 1).
In some patients, there is clinically significant inflammation, including effusions, warmth, and synovitis that is visible during surgery.
When osteoarthritis of the knee becomes severe, joint deformities — most commonly, varus (”bowlegs”) or valgus (”knock-knees”) — can occur.
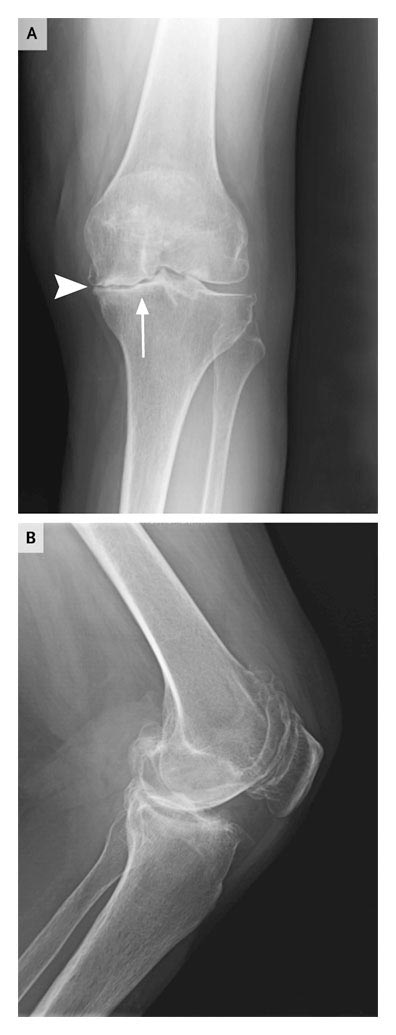
Figure 1. Radiograph of the Left Knee of a Patient with Osteoarthritis.
Panel A shows an anteroposterior view with visible eburnation of the subchondral bone (”sclerosis”) (arrow) and loss of articular surface cartilage (or joint-space narrowing) (arrowhead).
Panel B shows a lateral view, in which patellar osteophytes are also readily seen.
Total knee arthroplasty is an operation that consists of removal of the damaged cartilage, correction of joint deformities, and replacement of the worn cartilaginous bearing surfaces (on the femur, tibia, and patella) with an artificial bearing (Figure 2).
Arthroplasty is not a disease-modifying procedure but rather is a mechanical solution to a biologic problem.
 Figure 2. Radiograph of the Right Knee of a Patient after Total Knee Arthroplasty.
Figure 2. Radiograph of the Right Knee of a Patient after Total Knee Arthroplasty.
Shown are an anteroposterior view (Panel A) and a lateral view (Panel B) of the tibial components (arrows) and the femoral components (arrowheads).
For some patients with severe joint damage, arthroplasty may be the only option that offers the possibility of restored mobility and freedom from pain.
However, arthroplasty is a major operation, and recovery may be sometimes difficult.
Patients typically have substantial immediate postoperative pain, which must be tolerated if they DO NOT undergo the aggressive physical therapy that is supposed by too many notably medical (not surgical) authors to be required for a good outcome.
They do not very often use assistive devices for ambulation for more than 3 weeks (perhaps longer when contralateral knee is also worn out) and they do not require neither frequent physical therapy nor narcotic analgesics and in any case never for several months…12
Whatever the reasons, there is interest among surgeons and patients alike in methods that truely make total knee arthroplasty less “invasive”.13,14
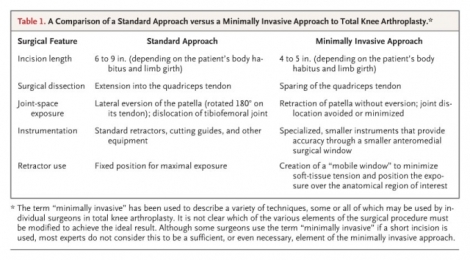
A variety of different procedures and techniques, all intended to reduce the amount of tissue injury occurring during surgery, are still lumped together under the label “minimally invasive surgery” (Table 1).
This general term is used to identify all such procedures in this review.
The purported advantages of minimally invasive approaches would include less postoperative pain, a shorter hospital stay, an earlier return of control for quadriceps muscles (leading to a shorter period of dependence on external devices for ambulation), and a briefer convalescence.12,13,14,15,16,17,18,19
There is limited evidence suggesting that minimally invasive total knee arthroplasty results in longer-term benefits in function than does the traditional approach,15,20.
Most surgeons think that any benefits that may accrue would be confined to the recuperative period.
Clinical Evidence
The clinical studies evaluating the potential benefit of minimally invasive total knee arthroplasty have a number of limitations.
Of the studies that have been conducted, very few are randomized, most are quite small, and some evaluate different methods or aspects of the minimally invasive approach, making a comparison among studies difficult.
Most of these studies do not take into account the skill development or “learning curve” of the surgeons who are performing the procedures.
In addition, all the studies have been performed in the context of the evolution of surgical practice.
In large measure because of these issues, there remains real conflict in the orthopedic literature about the benefit of this surgical approach.
In one of the few randomized trials, Kolisek et al.21 compared a minimally invasive approach with the traditional approach in 80 patients.
The investigators found no significant differences in clinical or radiographic results at 3 months of follow-up.
However, the authors defined “minimally invasive” surgery entirely as a function of incision length, since no specialized instruments were used in the group undergoing minimally invasive procedures, and the surgeons everted the patella (i.e., rotated it 180° on its tendon) as part of the operation.
The use of incision length alone, as in the study by Kolisek et al., is clearly not considered an appropriate or sufficient determinant to classify the procedure as minimally invasive (Table 1).
One of the largest nonrandomized studies22 involved 200 consecutive total knee arthroplasty operations (100 using the traditional approach and 100 using the minimally invasive approach), which were performed by experienced joint surgeons.
The investigators, McAllister and Stepanian, defined minimally invasive surgery as “total knee arthroplasty performed without dissection into the quadriceps tendon, eversion of the patella, or dislocation of the tibiofemoral joint; these operations also involved the use of instrumentation designed specifically for minimally invasive surgery.”
Patients who underwent the minimally invasive procedure had less postoperative pain and an improved early range of motion.
They also had a significantly decreased risk of requiring manipulation under anesthesia (14% vs. 2%, P<0.001), an additional procedure resulting from the failure of rehabilitation or pain control or other inexplained reason that might expose the patient to the risk of hemarthrosis, fracture, and tendon rupture.
In one study,12 were compared 100 minimally invasive procedures with 50 performed with the traditional approach.
The minimally invasive approach (with a definition very similar to that used by McAllister and Stepanian) would reduce the length of hospital stay from 3.7 to 2.8 days (P<0.001).
It would also significantly reduced the percentage of patients receiving narcotics at 2 weeks and at 6 weeks and the need for assistive devices for walking at 2 weeks.
Clinical Use
Regardless of whether total knee arthroplasty is performed through a traditional or minimally invasive approach, it may be a major surgical intervention, with all the attendant risks of surgery.
In addition, not all patients who undergo total knee arthroplasty have relief of symptoms even after a full recovery: 8 to 23% of patients have residual pain or stiffness in the knee at long-term follow-up.23
In light of these facts, it is prudent to exhaust reasonable nonsurgical alternatives before considering arthroplasty.
Nonsurgical interventions for pain associated with osteoarthritis of the knee include nonsteroidal antiinflammatory drugs, certain non-narcotic analgesics (in particular, acetaminophen), and intraarticular injections (corticosteroids or viscosupplements).24
It is reasonable to consider surgery when a patient, who is medically fit and is willing to accept the risks associated with the operation, has persistent, moderate-to-severe pain associated with activity despite nonsurgical interventions.
The patient should have radiographic evidence of significant joint damage, and if there appears to be inconsistency between the radiographic image and symptoms, I would consider other explanations for the patient’s pain.
Contraindications to total knee arthroplasty include active infection, thrombophilias, bleeding disorders, severe vascular disease or neurologic disease affecting sensory or motor function in the affected leg, and inadequate soft tissue to cover the joint.
An essential factor to take into account in considering surgery is the patient’s ability and willingness to participate, and a deleterious aggressive regimen of postoperative physical therapy is no substitute for good (gentle) surgical technique and patient empowerment.
Vigorous physical rehabilitation, including exercises specifically intended to require early and repetitive motion of the affected knee despite substantial pain, is NEVER necessary for a good result.
Failures of rehabilitation do not often stem from problems in managing postoperative pain early on, but from aggressive physical therapy or no patient empowerment at all, can permanently prejudice the outcome.25,26,27
Frequent communication with the surgeon should be the mainstay of these elderly patients empowerment.
Once the decision has been made to proceed with surgery, the discussion should not turn to whether a traditional or minimally invasive approach is more appropriate, or whether local or general anesthesia is preferred…
An essential factor to consider in this decision is the experience of the surgeon and the anesthesiologist and the qualification of this team.
In one study, is specifically evaluated the effect of experience and showed that a surgeon must typically perform 25 to 50 procedures using minimally invasive techniques before benefits of this approach can be expected.12
A fairly high practice volume is also important in maintaining the skills necessary for minimally invasive surgery, a principle that obviously applies to conventional surgery as well.28,29
Given the exclusion criteria of the major clinical studies, other relative contraindications to the minimally invasive approach may include previous open knee surgery,15,16,19,30,31 severe osteoporosis or rheumatoid arthritis,14,30,31 obesity or increased limb girth,12,14,15 and severe joint deformity.12,14
Anesthesia can be performed with the use of any of a variety of approaches.
Either general anesthesia or regional (spinal or epidural) anesthesia, with or without adjunctive peripheral-nerve block, is appropriate.
During the operation, the patient’s knee is typically positioned in some flexion, and tourniquet control is still unfortunately “used to reduce bleeding”.
The traditional approach uses an anterior longitudinal incision of 6 to 9 in. in length, whereas the minimally invasive approach often uses a somewhat shorter anteromedial incision along the medial border of the patella, extending distally to the level of the tibial tubercle.
The traditional approach may then involve a longitudinal incision through the quadriceps tendon; the minimally invasive approach opens the medial capsule and extends proximally and obliquely into either the midvastus plane or subvastus plane by a small amount (typically 1 to 3 cm) and avoids the quadriceps tendon (Figure 3).
In the traditional approach, the patella is then everted, whereas in the minimally invasive approach, the patella would be retracted laterally but not everted.
In the traditional approach, the tibiofemoral joint would be then dislocated and the knee hyperflexed.
In the minimally invasive approach, that joint would be left in situ without dislocation.
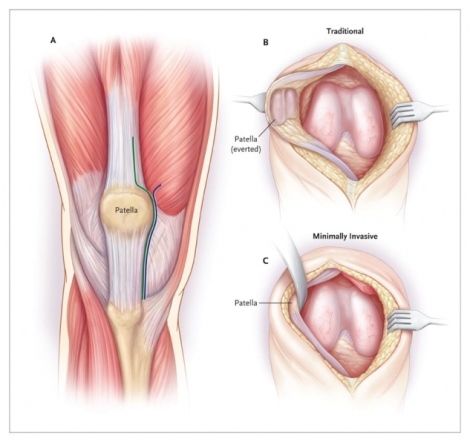
Figure 3. Elements of Minimally Invasive Total Knee Arthroplasty.
Panel A shows the anatomical relations of the deep-tissue surgical incision for total knee arthroplasty.
The traditional incision typically extends into the quadriceps tendon.
The minimally invasive incision spares the quadriceps tendon and extends into or beneath the vastus medialis muscle.
Joint-space exposure is shown for traditional total knee arthroplasty (Panel B) and for the minimally invasive procedure (Panel C).
In the traditional procedure, a larger incision is made, and retractors are placed in a fixed position for maximal exposure.
The tibiofemoral joint is dislocated, and the patella is everted (rotated laterally 180° on its tendon).
In the minimally invasive procedure, a relatively small incision is made, and retractors are shifted during surgery to create a “mobile window” for the minimum necessary exposure.
The tibiofemoral joint is not dislocated, and the patella is retracted laterally without being everted.
In both techniques, cutting jigs and anatomic landmarks are used to determine the depth and orientation of tibial and femoral bone resections.
In the minimally invasive procedure, the cutting guides are reduced in size, rounded, and designed to optimize accuracy through the smaller anteromedial window.
Regardless of approach, careful attention to ligament balancing and protecting neurovascular structures must be maintained.
Trial implants then are placed over the resected bone surfaces; joint stability, ligament balance, and range of motion then are assessed.
If satisfactory, final components are inserted (Figure 4).
Final hemostasis is then obtained, and the joint is irrigated and closed.
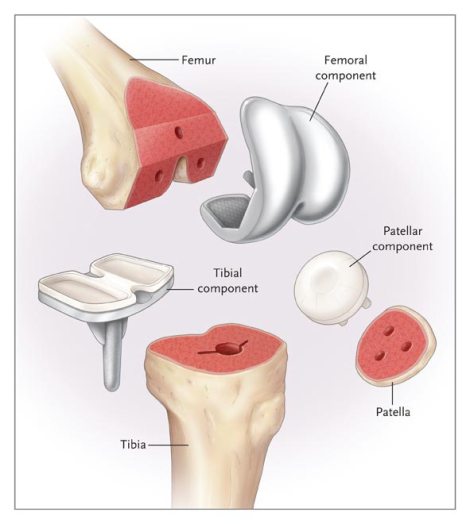
Figure 4. Components of Total Knee Arthroplasty.
Precise resections are made in the distal end of the femur, the proximal end of the tibia, and the posterior surface of the patella to fit the corresponding surfaces of the three arthroplasty components.
The femoral component is typically made of metal (most commonly, a cobalt–chromium alloy).
The patellar component is typically made of ultra-high-molecular-weight polyethylene (a plastic resin).
The tibial implant is usually made of metal (either a titanium or a cobalt–chromium alloy).
There is an exchangeable polyethylene bearing on the tibia, which therorically would make it possible to replace the plastic articular surface without replacing the metal component if (or at the time…) wear of the bearing surface occurs…
The period of convalescence varies.
As noted, in one study,12 the mean hospital stay for patients undergoing minimally invasive total knee arthroplasty is 2.8 days, about 1 day shorter than the mean duration for the traditional approach.
Physical therapy is NOT initiated the day of surgery, with no immediate emphasis on range of motion, gait training, safety, and transfers.
A machine that provides continuous passive motion may NOT be used to enhance the exercises performed with a physical therapist.32
Adequate analgesia during physical therapy would be essential and mandatory ; pain would be the most common threat to adequate progression of mobility.
In general, patients who have undergone minimally invasive total knee arthroplasty would require the use of a walker for about a week and the use of a cane for a week to 10 days, at which point unassisted ambulation might be the norm, should contralateral knee and back allow it…
Physical therapy usually would conclude by about 6 weeks with the minimally invasive approach; with the traditional approach, an additional month of therapy would usually be required.
Appropriate thromboprophylaxis is used after either traditional or minimally invasive surgery.
A variety of agents, including aspirin, warfarin, unfractionated heparin, and low-molecular-weight heparin, pentasaccharides are used for this purpose.
Intermittent pneumatic-compression devices that prevent venous stasis and that may enhance fibrinolysis commonly used in USA are no better than Tibialis Anterior and Vastus Medialis active exercises.
There is currently substantial disagreement between the recommendations of the American Academy of Orthopedic Surgeons and those of the American College of Chest Physicians regarding the appropriate intensity of anticoagulation.33,34
The same pertained between French surgeons and anesthésiologists before nerve blocks become fashionable (too much).
According to one study, the estimated mean cost of primary total knee arthroplasty was $29,290 on the basis of data collected from October 2005 through June 2006 at four high-volume centers.35
The study did not distinguish between the cost of minimally invasive procedures and that of traditional operations.
One expert observes that although the cost of minimally invasive total knee arthroplasty could be less than that of the conventional procedure (as a result of a shorter hospital stay), current reimbursement and global multidisciplinary policies may create incentives to keep the patient in the hospital longer.36
Adverse Effects
Many of the complications of total knee arthroplasty are similar whether a minimally invasive or traditional procedure is performed.
The most feared complication, infection of the joint, occurs in less than 1% of patients.37
By contrast, thromboembolic disease may be common even with appropriate thromboprophylaxis.
Venographic studies indicate that at least 15% of patients may have deep venous thrombosis, but symptomatic thromboembolic events occur in only 2 to 3% of patients.38
Nerve injuries, especially peroneal nerve palsy, occur in 1 to 2% of patients,39 whereas arterial vascular injury is much rarer.
As noted above, persistent pain or stiffness occurs in 8 to 23% of patients.23
Prosthesis failure, typically requiring surgical revision, occurs in approximately 2% of patients at 5 years.40
In some studies, specific problems associated with the minimally invasive approach include inferior mean alignment41 or an increased frequency of outliers in terms of alignment,41,42,43 concern about wound healing,21 a longer surgical duration,43 and an inability to validate claims regarding improvements in early recovery or the time to independent ambulation.21,42
However, most of these reports come from studies that enrolled patients early in the surgeon’s learning curve or that describe an approach as minimally invasive solely on the basis of the incision length.
For these reasons, the experience of the surgeon is an essential consideration in choosing minimally invasive total knee arthroplasty.
Areas of Uncertainty
As noted above, the designation “minimally invasive” total knee arthroplasty encompasses several different modifications in surgical technique.
It has not been established which of these changes are essential to improving outcomes for the patient.
Increasingly, all elements of the minimally invasive approach are being used together (Table 1).
It therefore seems unlikely that any trial will be conducted to distinguish, for example, the benefit of sparing the quadriceps tendon from that of avoiding or minimizing tibiofemoral-joint dislocation.
Since the minimally invasive approach has been in common use for less than 5 years, it has not yet been established that long-term outcomes will be as good (even in the hands of experienced surgeons) as those of patients undergoing traditional total knee arthroplasty.
Although the characteristics of the procedure itself do not suggest obvious grounds for concern in this regard, additional studies will be required to provide a definitive answer to this question.
A variety of further modifications of surgical technique have been described in the past few years.
These include computer-assisted navigation to aid in the precision of bone excision and prosthesis alignment, as well as recurrent interest in unicompartmental (partial) knee arthroplasty, meniscus replacement, and other similar elaborations, some of which are sometimes described as “minimally invasive” techniques.
The potential advantages of such approaches as compared with the operation outlined in this review of mine are not known.
Guidelines
There are no formal guidelines on the subject of minimally invasive total knee arthroplasty.
The American Academy of Orthopedic Surgeons offers only a brief comment on the guidelines page of its Web site and does not draw a distinction between minimally invasive total knee arthroplasty and minimally invasive total hip arthroplasty.
The hip procedure has provoked substantial controversy because of a high frequency of major complications.44,45
The group’s guidelines state that minimally invasive surgery for total joint replacement “is a promising, but evolving surgical technique that requires additional scientific evidence to validate its short- and long-term safety and effectiveness, in comparison to conventional joint replacement methods.”46
In 2004, the American Association of Hip and Knee Surgeons released an advisory statement about minimally invasive hip and knee arthroplasty that cites both potential advantages and disadvantages of the two approaches.47
Unfortunately, since most of the literature on minimally invasive total knee arthroplasty has been published since 2004, such statement is certainly out of date.
Recommendations
I do not know the “young and slim” patient who is described in the vignette (job ?, relatives ? mmpi ?), but she may be a suitable candidate for minimally total knee arthroplasty, however some further consideration of her specific circumstances is appropriate.
I would begin by discussing the major therapeutic options with the patient; in particular, I would try to ascertain whether she feels strongly that her quality of life with medical therapy alone has become unacceptable.
As her answer is probably yes (X rays ?), I would NOT describe the advantages and disadvantages of both the traditional and the minimally invasive approaches for total knee arthroplasty.
I would ONLY emphasize that either approach (minimally invasive approach or not) should be performed only by a surgeon with considerable expertise and experience.
I would describe the operation itself briefly but would place more emphasis on what she should expect in the perioperative and immediate postoperative period.
The patient should be informed that she would have substantial postoperative pain and that she would certainly need to participate actively but NOT in an aggressive regimen of physical therapy.
This kind of “aggressive regimen” is far from being mandatory to have a successful outcome: relief of symptoms and improvement in mobility and may even prove deleterious.
Referencess
- Buckwalter JA, Saltzman C, Brown T. The impact of osteoarthritis: implications for research. Clin Orthop Relat Res 2004;427:S6-S15. [CrossRef][Medline]
- Felson D. The epidemiology of osteoarthritis: prevalence and risk factors. In: Kuettner KE, Goldberg VM, eds. Osteoarthritic disorders. Rosemont, IL: The American Academy of Orthopaedic Surgeons, 1995:13-24.
- Praemer A, Furner S, Rice DP. Musculoskeletal conditions in the United States. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1999.
- Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Surgery 1991-94. J Rheumatol 2006;33:2271-2279. [Free Full Text]
- WHO, Bone and Joint Decade. The global economic and healthcare burden of musculoskeletal disease. Geneva: World Health Organization, 2001. (Available at http://www.boneandjointdecade.org/.)
- Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 2000;133:635-646. [Free Full Text]
- Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol 2007;213:626-634. [CrossRef][ISI][Medline]
- Goldring SR, Goldring MB. The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin Orthop Relat Res 2004;427:Suppl:S27-S36. [CrossRef][Medline]
- Fukui N, Purple CR, Sandell LJ. Cell biology of osteoarthritis: the chondrocyte’s response to injury. Curr Rheumatol Rep 2001;3:496-505. [Medline]
- Lohmander LS, Atley LM, Pietka TA, Eyre DR. The release of crosslinked peptides from type II collagen into human synovial fluid is increased soon after joint injury and in osteoarthritis. Arthritis Rheum 2003;48:3130-3139. [CrossRef][ISI][Medline]
- Felson DT. Risk factors for osteoarthritis: understanding joint vulnerability. Clin Orthop Relat Res 2004;427:Suppl:S16-S21. [CrossRef][Medline]
- King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty: assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am 2007;89:1497-1503. [Free Full Text]
- Bonutti PM, Mont MA, McMahon M, Ragland PS, Kester M. Minimally invasive total knee arthroplasty. J Bone Joint Surg Am 2004;86:Suppl 2:S26-S32.
- Tria AJ Jr, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res 2003;416:185-190. [CrossRef][Medline]
- Haas SB, Cook S, Beksac B. Minimally invasive total knee replacement through a mini midvastus approach: a comparative study. Clin Orthop Relat Res 2004;428:68-73. [CrossRef][Medline]
- Laskin RS, Beksac B, Phongjunakorn A, et al. Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res 2004;428:74-81. [CrossRef][Medline]
- Seon JK, Song EK. Navigation-assisted less invasive total knee arthroplasty compared with conventional total knee arthroplasty: a randomized prospective trial. J Arthroplasty 2006;21:777-782. [CrossRef][ISI][Medline]
- Seon JK, Song EK, Yoon TR, Park SJ, Bae BH, Cho SG. Comparison of functional results with navigation-assisted minimally invasive and conventional techniques in bilateral total knee arthroplasty. Comput Aided Surg 2007;12:189-193. [CrossRef][ISI][Medline]
- Song EK, Seon JK, Yoon TR, Park SJ, Bae BH, Cho SG. Functional results of navigated minimally invasive and conventional total knee arthroplasty: a comparison in bilateral cases. Orthopedics 2006;29:Suppl 10:S145-S147. [Erratum, Orthopedics 2007;30:327.] [ISI][Medline]
- Flören M, Davis J, Peterson MG, Laskin RS. A mini-midvastus capsular approach with patellar displacement decreases the prevalence of patella baja. J Arthroplasty 2007;22:Suppl 2:S51-S57. [CrossRef]
- Kolisek FR, Bonutti PM, Hozack WJ, et al. Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. J Arthroplasty 2007;22:8-13. [ISI][Medline]
- McAllister CM, Stepanian JD. The impact of minimally invasive surgical techniques on early range of motion after primary total knee arthroplasty. J Arthroplasty 2008;23:10-18. [CrossRef][ISI][Medline]
- Lingard EA, Sledge CB, Learmonth ID. Patient expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am 2006;88:1201-1207. [Free Full Text]
- The Cochrane Collaboration home page. (Accessed March 30, 2009, at http://www.cochrane.org.)
- Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW. Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 1996;11:831-840. [CrossRef][ISI][Medline]
- Maloney WJ. The stiff total knee arthroplasty: evaluation and management. J Arthroplasty 2002;17:Suppl 1:S71-S73. [CrossRef]
- Walton NP, Jahromi I, Dobson PJ, Angel KR, Lewis PL, Campbell DG. Arthrofibrosis following total knee replacement: does therapeutic warfarin make a difference? Knee 2005;12:103-106. [CrossRef][ISI][Medline]
- Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R. Provider volume of total knee arthroplasties and patient outcomes in the HCUP-Nationwide Inpatient Sample. J Bone Joint Surg Am 2003;85:1775-1783. [Free Full Text]
- Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am 2004;86:1909-1916. [Free Full Text]
- Tashiro Y, Miura H, Matsuda S, Okazaki K, Iwamoto Y. Minimally invasive versus standard approach in total knee arthroplasty. Clin Orthop Relat Res 2007;463:144-150. [Medline]
- Lombardi AV Jr, Viacava AJ, Berend KR. Rapid recovery protocols and minimally invasive surgery help achieve high knee flexion. Clin Orthop Relat Res 2006;452:117-122. [CrossRef][Medline]
- Milne S, Brosseau L, Robinson V, et al. Continuous passive motion following total knee arthroplasty. Cochrane Database Syst Rev 2003;2:CD004260-CD004260. [Medline]
- American Academy of Orthopaedic Surgeons. Clinical guideline on prevention of pulmonary embolism in patients undergoing total hip or knee arthroplasty. (Accessed March 30, 2009, at http://www.aaos.org/research/guidelines/PE_guideline.pdf.)
- Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 2008;133:6 Suppl:381S-453S. [CrossRef][ISI][Medline]
- Bozic KJ, Rubash HE, Sculco TP, Berry DJ. An analysis of medicare payment policy for total joint arthroplasty. J Arthroplasty 2008;23:Suppl 1:S133-S138. [CrossRef]
- Bozic KJ, Hansen E. The economics of minimally invasive total knee arthroplasty. J Knee Surg 2006;19:149-152. [Medline]
- Jämsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors for infection after knee arthroplasty: a register-based analysis of 43,149 cases. J Bone Joint Surg Am 2009;91:38-47. [Free Full Text]
- Douketis JD, Eikelboom JW, Quinlan DJ, Willan AR, Crowther MA. Short-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of prospective studies investigating symptomatic outcomes. Arch Intern Med 2002;162:1465-1471. [Free Full Text]
- Schinsky MF, Macaulay W, Parks ML, Kiernan H, Nercessian OA. Nerve injury after primary total knee arthroplasty. J Arthroplasty 2001;16:1048-1054. [CrossRef][ISI][Medline]
- Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat Award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res 2006;452:28-34. [CrossRef][Medline]
- Chin PL, Foo LS, Yang KY, Yeo SJ, Lo NN. Randomized controlled trial comparing the radiologic outcomes of conventional and minimally invasive techniques for total knee arthroplasty. J Arthroplasty 2007;22:800-806. [CrossRef][ISI][Medline]
- Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res 2005;440:77-81. [CrossRef][Medline]
- Huang HT, Su JY, Chang JK, Chen CH, Wang GJ. The early clinical outcome of minimally invasive quadriceps-sparing total knee arthroplasty: report of a 2-year follow-up. J Arthroplasty 2007;22:1007-1012. [CrossRef][ISI][Medline]
- Bal BS, Haltom D, Aleto T, Barrett M. Early complications of primary total hip replacement performed with a two-incision minimally invasive technique. J Bone Joint Surg Am 2005;87:2432-2438. [Free Full Text]
- Pagnano MW, Leone J, Lewallen DG, Hanssen AD. Two-incision THA had modest outcomes and some substantial complications. Clin Orthop Relat Res 2005;441:86-90. [CrossRef][Medline]
- American Academy of Orthopaedic Surgeons. Clinical practice guidelines: advisory statement. (Accessed March 30, 2009, at http://www.aaos.org/Research/guidelines/guide.asp.)
- American Association of Hip and Knee Surgeons. Physician advisory statement: minimally invasive and small incision joint replacement surgery: what surgeons should consider. (Accessed March 30, 2009, at http://www.aahks.org/member/resources/MIS_Surgeons.pdf.)
Leave a comment